Facial Bone The function of the facial bone is to protect our brain and other sensitive organs situated in our face like an organ of ...
View AllCT SCAN
View AllMRI Case
1
The First World's Color Xray Image
Saturday, September 29, 2018
A father and son tandem from New Zealand has introduced the first ever colored x-ray scanner adapted from technology used in finding th...
2
UK’s first MR Linac, combining MRI and radiotherapy technology
Thursday, September 27, 2018
The first MR linac to be commissioned in the UK is starting to be used to treat patients. The benefit of the Elekta Unity magnetic...
0
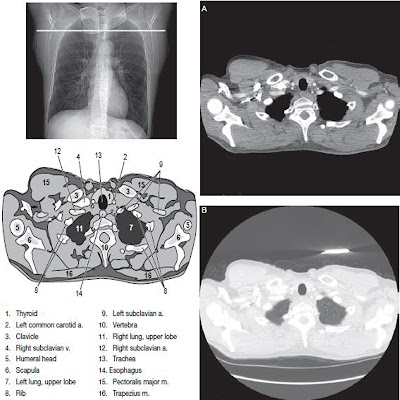
Computed Tomography of the Brain
Tuesday, September 25, 2018
CT Scan of the Brain Indications CT is the imaging modality most commonly used in triaging acute neurological disease. For non em...
0
Methods of Radiographic Imaging the Brain
Tuesday, September 18, 2018
Imaging the brain’s structure and examining its physiology, both in the acute and elective setting, are now the domain of multiplanar, comp...
Subscribe to:
Posts (Atom)